State Health Assessment shows progress on oral health in Ohio
The Health Policy Institute of Ohio recently released the “State Health Assessment for Ohio.” The report shows significant progress is being made in the area of oral health but that more needs to be done to address oral health disparities by race and geography.
The Ohio Department of Health contracted with the Health Policy Institute of Ohio to perform the assessment, which was conducted from March to July 2016. The State Health Assessment is a comprehensive picture of overall health and wellbeing in Ohio. Oral health was only a small part of the State Health Assessment, but the final report provides some valuable information on the progress that is being made.
 Children with Unmet Dental Needs
Children with Unmet Dental Needs
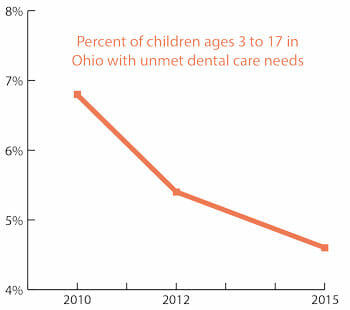
According to the State Health Assessment report, “the percent of children with unmet dental-care needs decreased,” continuing a trend that began in 2012. Specifically, the State Health Assessment found that the percent of children ages 3 to 17 with unmet dental care needs decreased from 6.8 percent in 2010 to 5.4 percent in 2012 and 4.6 percent in 2015, a more than 30 percent decline over the five year period.
 Adult Dental Visits
Adult Dental Visits
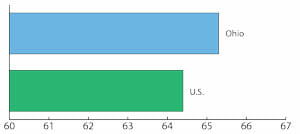
Ohio also fares well on adult oral health. For example, according to the State Health Assessment report, 65.3 percent of adults visited a dentist or dental clinic within the previous 12 months, which was above the national average of 64.4 percent.
Population to Dentist Ratio
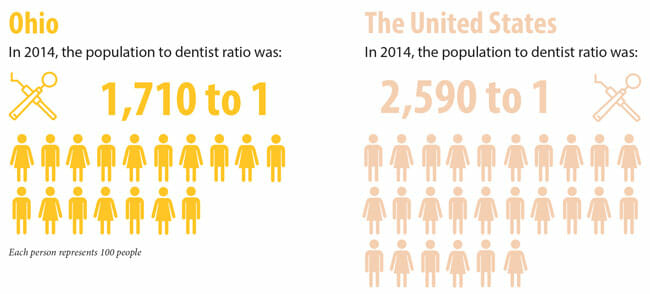
The State Health Assessment also demonstrates that Ohio’s dentist workforce is larger than the typical state and is growing even when adjusted for population growth. For example, in 2012, the population to dentist ratio in Ohio was 1,789 to one. In 2013, it was 1,746 to one and in 2015 (the most recent year measured) the population to dentist ratio was down to 1,710 to one. Ohio fares much better than the national average in population to dentist ratio, which is 2,590 to one.
Disparities in Oral Health
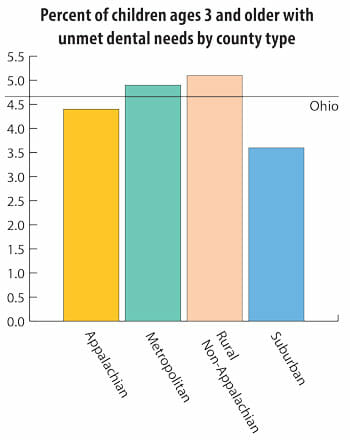 While the State Health Assessment revealed much good news about oral health demonstrating that Ohio is making progress and is doing better than many other states in important oral health indices, the report also revealed that there are disparities in oral health by race and geography. For example, while statewide workforce ratios show that Ohio performs better than the U.S. average, there are certain areas of the state where unmet dental needs persist. The report notes that Ohio had a slightly higher percentage of its population living in an area underserved for dental care than the national average. Children living in suburban areas were least likely to experience unmet dental care needs, while children living in rural and metropolitan areas were more likely to experience unmet dental care needs. Hispanic and African-American children were more likely to experience unmet dental care needs when compared to Ohioans who identified as white or other.
While the State Health Assessment revealed much good news about oral health demonstrating that Ohio is making progress and is doing better than many other states in important oral health indices, the report also revealed that there are disparities in oral health by race and geography. For example, while statewide workforce ratios show that Ohio performs better than the U.S. average, there are certain areas of the state where unmet dental needs persist. The report notes that Ohio had a slightly higher percentage of its population living in an area underserved for dental care than the national average. Children living in suburban areas were least likely to experience unmet dental care needs, while children living in rural and metropolitan areas were more likely to experience unmet dental care needs. Hispanic and African-American children were more likely to experience unmet dental care needs when compared to Ohioans who identified as white or other.
Reasons for Progress
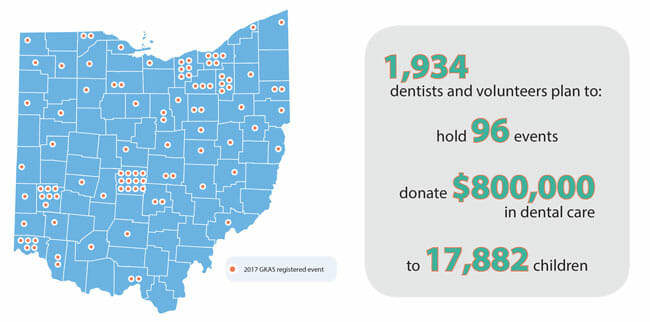
There are many reasons for Ohio’s progress. Ohio has been proactive in creating a positive environment for improving access to dental care. Ohio dentists’ volunteerism is having a positive impact. The ODA’s Give Kids a Smile program is celebrating its 15th anniversary. In 2017, nearly 2,000 dentists and other volunteers are participating in events at 96 different sites across Ohio seeing nearly 18,000 Ohio kids and providing more than $800,000 in free care. Since the GKAS program’s kickoff 15 years ago, ODA member dentists have provided care to more than 236,000 Ohio children donating services worth more than $12.6 million.
Similarly, ODA member dentists have provided on average more than $1 million annually in dental services in recent years through the Dental OPTIONS program, which matches low income Ohioans with dentists who provide free or reduced fee dental care. Give Kids a Smile and the Dental OPTIONS program are just two examples of the many ways Ohio dentists provide free care to Ohioans. In fact, a recent independent survey of ODA members conducted by Saperstein Associates demonstrates that Ohio dentists donate a total of more than $40 million in dental care annually.
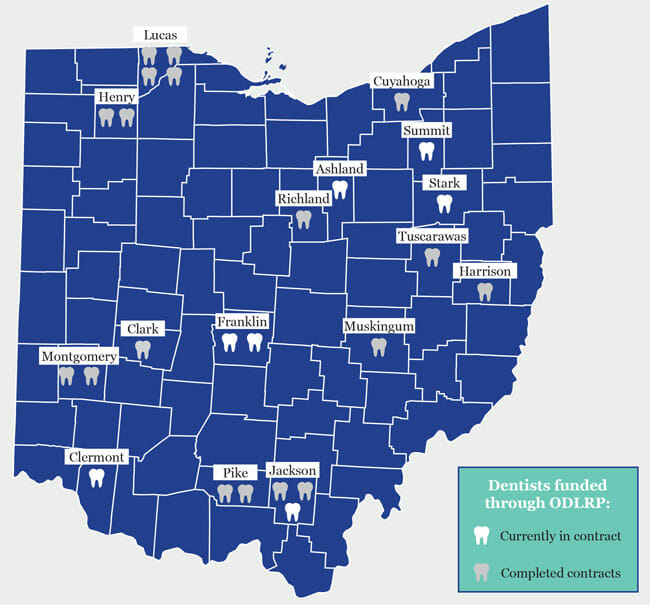 The ODA has been proactive in creating a positive environment for improving access to dental care through its advocacy. In the last decade, the ODA’s advocacy led to the creation of the Ohio Dentist
The ODA has been proactive in creating a positive environment for improving access to dental care through its advocacy. In the last decade, the ODA’s advocacy led to the creation of the Ohio Dentist
Loan Repayment Program, which is entirely funded by a surcharge on dentists’ license fees. This program has created incentives resulting in dozens of dentists relocating to designated dental professional shortage areas and providing care to the underserved.
In 2010, the ODA worked to pass legislation reestablishing the school-based fluoride rinse program, providing much needed prevention to underserved school children, and created the oral health access supervision program, allowing dentists to authorize their dental hygienists to provide prevention services to underserved patients in public health settings.
In 2014, the ODA worked to pass legislation to make dental education eligible for Choose Ohio First scholarships and to further enhance the ability of dental team members – including dental hygienists, expanded function dental assistants, and certified dental assistants – to deliver prevention services, including dental sealants, fluoride varnish, and oral health education, in many community settings, including schools and nursing homes. In 2015, the ODA also worked with the General Assembly and Kasich administration to increase funding for the dental Medicaid program.
The expansion of the dental safety net has also contributed to the positive momentum in improving access to dental care. In recent years, dozens of new dental clinics have been established, including federally qualified health centers and new dental residency programs, which have become important parts of the dental safety net in many Ohio communities.
 Ohio’s dental schools have also demonstrated a commitment to ensuring their students are involved in providing care to underserved patients and in the process enhancing the students’ social and cultural awareness. Through the Ohio State University College of Dentistry’s Oral Health Improvement through Outreach (OHIO) Project, fourth-year dental students spend 50 days providing care in community clinics throughout Ohio under the supervision of associated faculty and alumni.
Ohio’s dental schools have also demonstrated a commitment to ensuring their students are involved in providing care to underserved patients and in the process enhancing the students’ social and cultural awareness. Through the Ohio State University College of Dentistry’s Oral Health Improvement through Outreach (OHIO) Project, fourth-year dental students spend 50 days providing care in community clinics throughout Ohio under the supervision of associated faculty and alumni.
Through the Case Western Reserve School of Dental Medicine’s Healthy Smiles Sealant Program, dental students provide exams and sealants to students in all of the elementary schools in the Cleveland Metropolitan School District. The Case dental sealant program is an important adjunct to the Ohio Department of Health’s School-based Sealant Programs, which provide prevention services to thousands of high-risk Ohio school children.
The ODA also partners with interested parties, including the Ohio Association of Community Health Centers, Nationwide Children’s Hospital, Dental Center of Northwest Ohio, American Academy of Pediatrics, Ohio Association of School Nurses, and others, as part of the Children’s Oral Health Action Team. COHAT actively promotes prevention, oral health awareness, and interdisciplinary cooperation around oral health issues.
The Future
While the State Health Assessment provides validation that Ohio is making progress in improving access to dental care, it also identifies areas for improvement, especially related to oral health disparities. We know that there are still pockets of Ohioans who would benefit from expansion of our current efforts to provide high quality dental care. As we have consistently done throughout our 150 year history, the ODA will continue to find innovative solutions to ensure all Ohioans have access to the full range of oral health services that only a dentist is trained to provide.
The ODA is working with the General Assembly to pass legislation effectively doubling the capacity of the Ohio Dentist Loan Repayment Program, which creates incentives for dentists to provide care to underserved populations in designated dental professional shortage areas in urban and rural communities. Again, this program and its expansion are entirely funded by Ohio’s dentists. The legislation will also update Ohio’s laws to permit dentists to utilize tele-dentistry to extend the reach of the dental team into underserved communities to provide valuable prevention and other oral health services and to expand the ability of existing dental team members to provide care to the fullest extent of their training. The bill will also target specific scholarships in the Choose Ohio First Program for dental students who agree to practice in designated underserved areas in Ohio upon graduation.
As part of its major new building renovation, the Ohio State University College of Dentistry is in the process of expanding its class size by nearly 10 percent, which will mean that 40 more dental students will be getting trained at OSU’s dental school when the expansion is fully implemented. These new seats – 10 in each class – will be reserved specifically for Ohioans from designated dental professional shortage areas.
Moving forward, many of these solutions – loan repayment, Choose Ohio First scholarships, expansion of the dental school class at the Ohio State University College of Dentistry, better use of tele-dentistry – will specifically help address those disparities in oral health care identified in the State Health Assessment.
There is one more solution that is absolutely critical for addressing access to dental care in Ohio: Medicaid reform. According to research from the American Dental Association’s Health Policy Institute, Ohio ranks 41st out of 50 states in terms of Medicaid reimbursement for dental services. On average, Medicaid reimburses at about 40 percent of a dentists’ regular fee for most procedures.
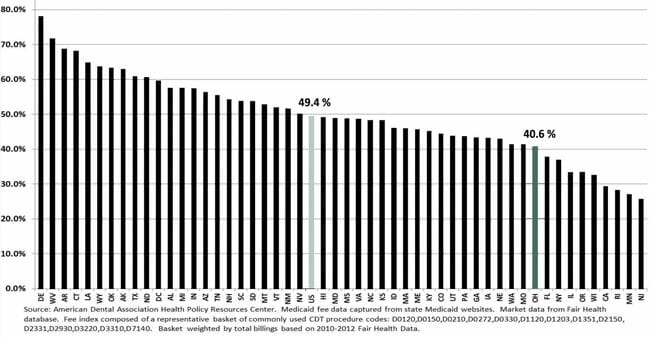
Over the last 17 years, Ohio’s dental fees have only been adjusted just once, in 2016, to increase reimbursements for extractions and denture repairs statewide and a 5 percent fee increase for all dental procedures in 52 rural counties. While this adjustment was welcome, the reality is that Medicaid dental reimbursements have fallen to levels that make it extremely difficult for dentists to participate as providers in the Medicaid program.
This situation cannot continue if the dental Medicaid program in Ohio is going to remain viable. A recent ADA report found that only about a third of Ohio’s dentists participate in the Medicaid program. In states that have increased dental Medicaid reimbursements closer to market levels, more dentists treat Medicaid patients and Medicaid patients have demonstrably better access to care. For example, a recent study analyzing Medicaid utilization following reimbursement rate increases in Connecticut, Maryland and Texas concluded that “increasing Medicaid dental fees closer to private insurance fee levels has a significant impact on dental care utilization and unmet dental need among Medicaid-eligible children.” Ohio policymakers can largely resolve access to dental care issues by following the lead of those states that have fixed their dental Medicaid programs, including by raising fees closer to market rates.
